Abstract
Introduction : Testing for monoclonal proteins may be undertaken as part of the diagnostic evaluation for chronic kidney disease. However, the clinical significance of monoclonal gammopathy detected in this context is often uncertain. Here we examined the association of a positive test for monoclonal protein with progression to end-stage renal disease (ESRD) (dialysis or kidney transplant) among United States (US) veterans.
Methods : We used national Veterans Health Administration (VA) clinical and administrative data to identify and characterize a national cohort of veterans with at least one serum creatinine measurement within the VA between October 1, 2000 and September 30, 2001. We used a text search algorithm for keywords pertaining to monoclonal protein contained in laboratory test results in the VA Corporate Data Warehouse within a two-year window of serum creatinine measurement to identify cohort members who had at least one test for monoclonal proteins (serum protein or urine electrophoresis or immunofixation), and to score test results as positive, negative, or unclassifiable. The text-search algorithm was validated by manual review of a random selection of 2% of records (training set) by an attending hematologist. A second manual review of a random selection of 737 records provided a validation set for the search algorithm, demonstrating a sensitivity of 0.73 (95% confidence interval (CI)) of 0.66-0.79, and specificity of 0.94 (95% CI 0.91-0.96), excluding unclassifiable tests. Patients were followed from the time of their first serum creatinine measurement during fiscal year 2001 through September 30, 2011 for the outcome of ESRD using linked data from the US Renal Data System, a national registry for ESRD. Cox proportional hazards regression stratified by glomerular filtration rate (eGFR ml/min/1.73 m2) was used to estimate hazard ratios (HR) with 95% CI for ESRD for patients with a positive vs. negative paraprotein test adjusted for age, sex, race, diabetes, congestive heart failure, vascular disease, and Charlson comorbidity index.
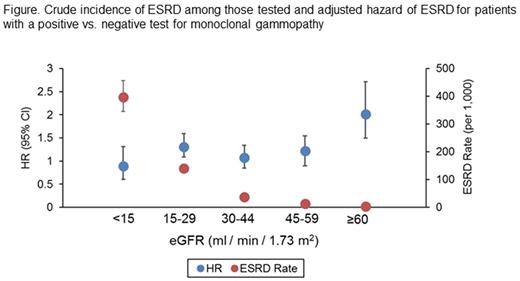
Results : Among a cohort of over 2.1 million veterans with a serum creatinine test, we identified 19,993 who underwent paraprotein testing. Overall, 96% of the cohort were male, 69% were ≥ 55 years old, and 23% were ≥ 75 years old. Of those tested, 4,112 (20.5%) had a positive test, 14,541 had a negative test (72.7%) and 6.7% were unclassifiable. Among those with an eGFR <60, 2% (n=8,293) underwent paraprotein testing, as compared with 0.7% (N=11,700) of those with an eGFR≥60. For all levels of eGFR, the crude incidence of ESRD was higher among patients who were tested vs. not tested. For patients with eGFR ≥60 who underwent testing for monoclonal gammopathy, there was an increased crude rate of ESRD among those with a positive vs. negative test result (4.9 vs 2.2 per 1,000 person years) with an adjusted HR of 2.01 (95% CI 1.50-2.71). For patients with lower levels of eGFR, in whom the absolute rate of ESRD was much higher, the adjusted HR for ESRD for those with a positive vs negative test result was attenuated and varied little by eGFR (Figure).
Conclusions : Among a large national cohort of US veterans, the risk of progression to ESRD in patients with a reduced eGFR who were tested for monoclonal gammopathy was similar regardless of whether the test result was positive or negative. Although there was an increased risk of ESRD among patients with preserved eGFR, the absolute risk of ESRD in these patients was very low. Evaluating different paraprotein sub-types and correlation with quantitative test results, including serum free light chain (kappa/lambda) ratios may further improve assessment of renal prognosis in patients with monoclonal gammopathy.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal